In the past, standard dental restorative materials were metals such as amalgam, gold or non-precious alloys with high atomic numbers. These metals – i.e. titanium, copper, strontium, ytterbium, silver, gold, bromine, barium, and strontium – are radiopaque and easily block out x-rays. This enables dental professionals to identify materials containing these elements on radiographs.
Radiopacity has thus become a very important property for dental restorations. It not only helps diagnose defects such as fractures, voids, over contouring, missing proximal contact, marginal imperfections, secondary caries and more, but it’s also helpful in documenting treatment for dental insurance reimbursement.
Even if natural hard dental substances do not contain highly radiopaque chemical elements, they still offer a certain degree of radiopacity. This is due to the calcium and phosphorus in their inorganic component, the hydroxylapatite. These elements are more concentrated in enamel than in dentin, making enamel more radiopaque than dentin. During the caries process, bacteria-produced acids cause hydroxylapatite to be released from the dental tissues, which is why carious lesions appear less radiopaque than intact enamel or dentin.
Radiopacity in modern dental restorative materials
Over the last few decades, metallic restorative materials have been increasingly replaced by esthetic resin-based composites as well as full ceramic materials. Originally, these composite materials did not contain any radiopaque chemical elements. This is why the first generations of composite resins, classified as conventional macro-filled and as microfilled composites, displayed a very low radiopacity or no radiopacity at all. The same was true for the first generation of full ceramic feldspathic porcelain restorative materials. At the time, this absence of radiopacity was not important, because these materials were primarily used for anterior restorations. Anterior restorations are monitored clinically without the help of radiographs, unlike posterior restorations where bite wing X-rays are routinely used.
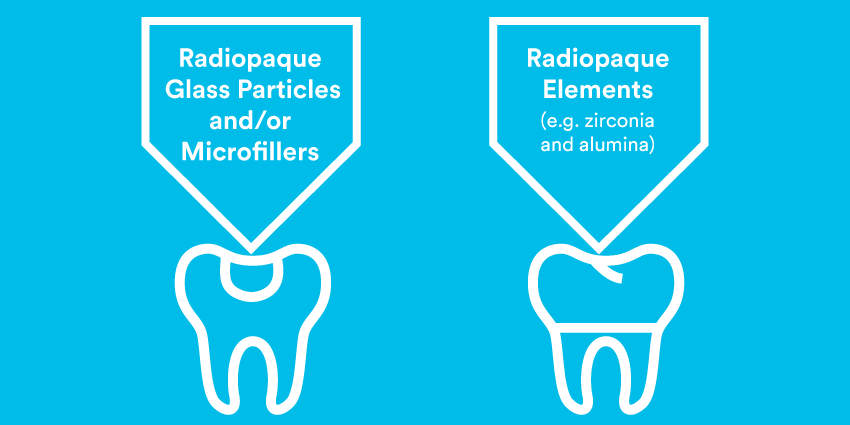
As soon as dentists started to use composites and full ceramic restorations in posterior teeth, radiopacity became of paramount importance and manufacturers were obliged to find ways to introduce radiopaque elements into their materials.1 Composite resins are composed of organic resins and reinforcing inorganic particles. To make the resin portion of a composite radiopaque is challenging, as resins typically contain chemical elements with low atomic numbers, such as hydrogen, oxygen, carbon or nitrogen. For this reason, composite resin manufacturers preferred to achieve adequate radiopacity by incorporating radiopaque glass particles – such as barium, strontium and zirconia atoms, or microfillers containing yttrium and ytterbium – into their formulations. Manufacturers of full ceramic materials, on the other hand, made use of different chemical elements with high atomic numbers, such as zirconia and alumina, in the crystalline ceramic phase. These additions ultimately solved the radiopacity issue for esthetic metal-free restorative materials.
Radiopacity in dental adhesives
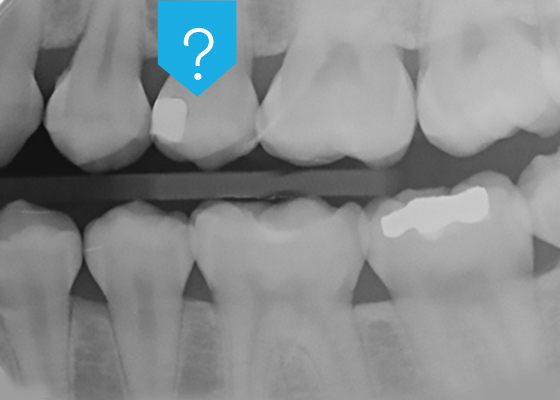
As esthetic restorations are increasingly bonded to the tooth with the help of universal adhesive systems, an important problem has remained unresolved: universal adhesives are radiolucent.
A radiolucent adhesive makes it impossible to differentiate between adhesive pooling and secondary caries, marginal gaps or voids beneath the restoration, particularly in difficult-to-inspect areas. Very experienced practitioners may try to distinguish between secondary caries and the adhesive layers by taking the morphology of the radiolucency into consideration, but it remains an educated guess with no guarantee. To be 100% sure, and to avoid legal problems, many practitioners prefer to replace the restoration entirely, which may end up being completely unnecessary. In these cases, radiopacity is clearly a desirable property for dental adhesives.
These adhesives are made with radiolucent resins and include a nominal amount of fillers to adjust consistency. However, adding radiopaque inorganic fillers into the resin matrix may lead to a paste-like consistency – which is unfavorable to the wetting and penetration properties of a one-component adhesive. And if the viscosity of the rest of the formulation is decreased, it can lead to separation and settling of the filler particles, which could make the mixture inhomogeneous and unstable during storage.
Overcoming the challenge
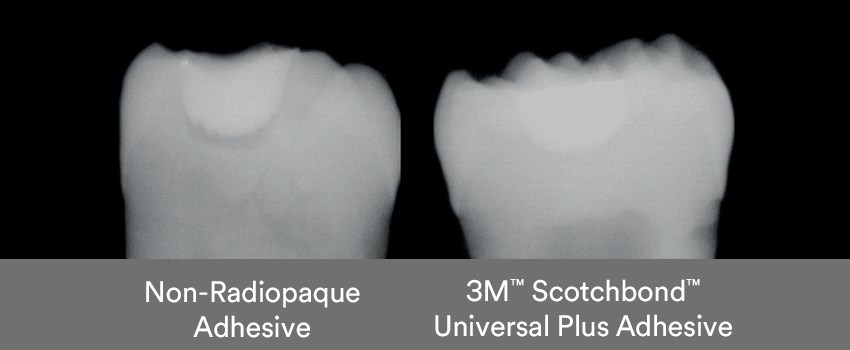
3M took on the challenge and developed a new radiopaque monomer, free of BPA derivatives like BisGMA, to solve the problem of radiolucency for universal adhesive systems. This novel monomer is based on the introduction of radiopaque building blocks into the molecular structure – and represents a breakthrough in adhesive dentistry. For the first time ever, dental professionals can utilize a one-component universal adhesive system with consistent performance, low viscosity and a desired radiopacity.
This new universal adhesive’s radiopacity is comparable to that of sound, non-demineralized dentin.2 It is also in line with ISO 4049, which specifies that the radiopacity of restorative materials should be at least as high as the radiopacity of aluminum of the same thickness.3 This makes it possible to make a clear distinction between secondary caries, marginal gaps or voids and the adhesive layer in a clinical setting.

Conclusion
The new radiopaque universal adhesive may reduce the risk of misinterpreting thick adhesive layers as secondary caries, marginal gaps or voids beneath composite or ceramic restorations on radiographs – thereby helping avoid unnecessary overtreatment and ultimately improve the quality of restorative dental treatments.
Sources
1. Hitij T, Fidler A: Radiopacity of dental restorative materials. Clin Oral Invest 17:1167-1177, 2013
2. H. Loll, O. Brinkmann, B. Anich, K. Dede, B., Craig, A.S. Abuelyaman, C. Thalacker. Radiopacity of an experimental universal adhesive, J Dent Res 99 (Spec Iss A):191, IADR, 2020
3. International Standards Organization ISO 4049: Dentistry – polymer-based restorative materials, 5th edt., ISO, Geneva, 2019

